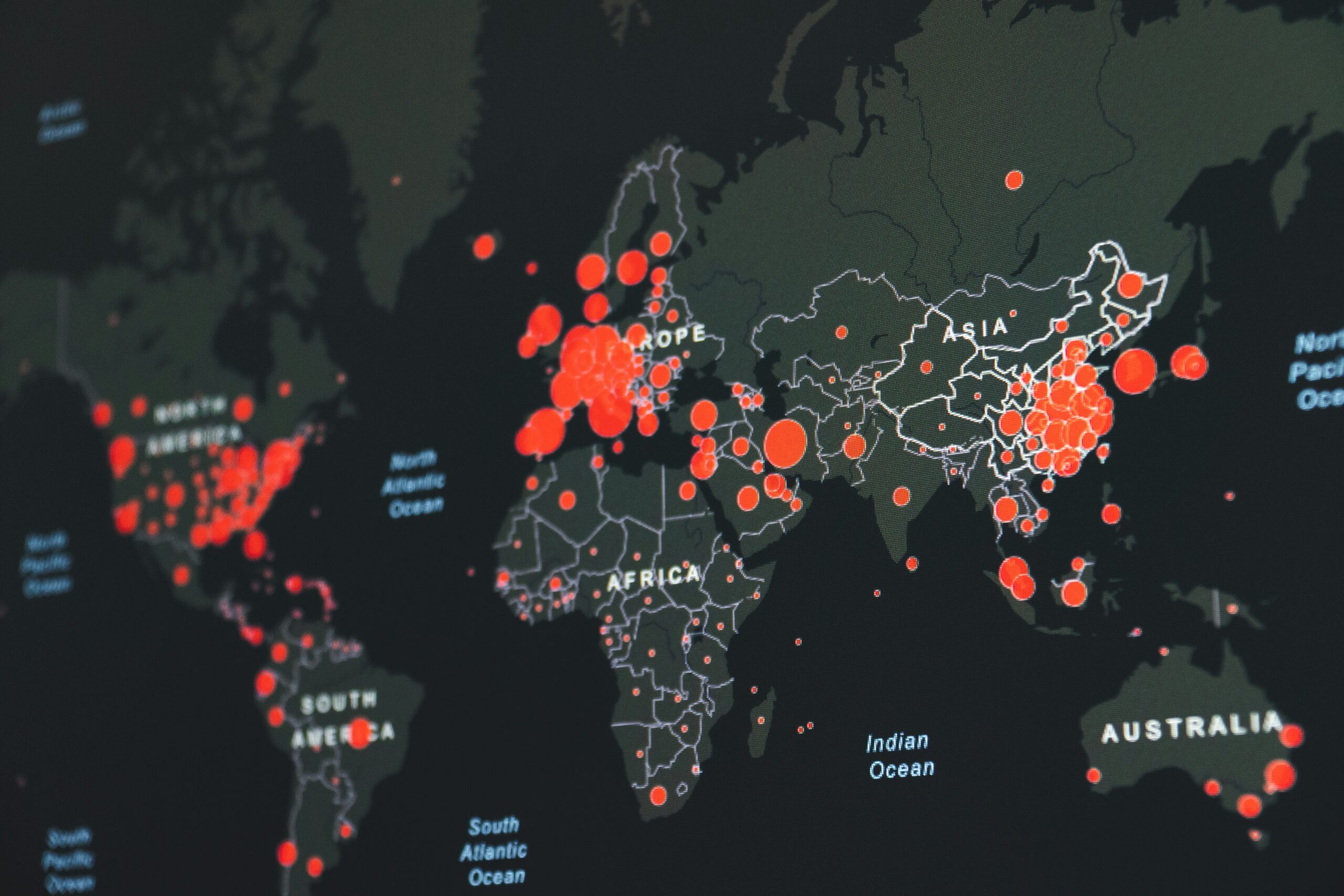
Antimicrobial resistance is emerging as a silent pandemic, posing a significant threat to global health. As bacteria, viruses, fungi, and parasites evolve to resist the drugs designed to kill them, common infections and minor injuries once easily treated become increasingly deadly. The World Health Organization (WHO) warns that without urgent action, AMR could lead to millions of deaths annually by 2050.
The rise of antimicrobial resistance is primarily driven by the overuse and misuse of antibiotics in humans and animals, as well as poor infection control practices. Inadequate sanitary conditions, lack of clean water, and insufficient access to healthcare further exacerbate the spread of resistant pathogens. The agricultural sector’s routine use of antibiotics to promote animal growth and prevent disease also contributes significantly to this global health crisis.
Addressing antimicrobial resistance requires a multifaceted approach, including public awareness campaigns, stricter regulations on antibiotic use, and robust infection prevention and control measures. Research and development of new antibiotics and alternative treatments are equally crucial. Healthcare professionals play a pivotal role in educating patients about the importance of using antibiotics responsibly and only when prescribed by a qualified healthcare provider.
Global collaboration is essential in the fight against antimicrobial resistance. International organizations, governments, healthcare institutions, and individuals must work together to implement effective strategies to combat this threat. By understanding the causes and consequences of AMR and taking proactive steps to mitigate its impact, we can protect the health of future generations and ensure that effective treatments remain available for all.
Table of Contents
The Rise of Antimicrobial Resistance
Antimicrobial resistance has become a significant global health threat, emerging from a combination of factors that have collectively fostered an environment where pathogens can thrive despite medical interventions. Understanding these factors is crucial to developing strategies to combat AMR effectively.

Causes and contributing factors
The primary causes of antimicrobial resistance include the overuse and misuse of antibiotics, poor infection control practices, and inadequate sanitation. These factors create a breeding ground for resistant bacteria, leading to the ineffectiveness of standard treatments and increasing the spread of resistant strains.
Overuse and Misuse of Antibiotics
One of the main drivers of antimicrobial resistance is the overuse and misuse of antibiotics in both human medicine and agriculture. In human healthcare, antibiotics are often prescribed for viral infections, against which they are ineffective, or patients may not complete their prescribed course, allowing resistant bacteria to survive and multiply. In agriculture, the routine use of antibiotics to promote growth in livestock further accelerates the development of resistance.
Impact of Poor Infection Control Practices
Poor infection control practices in healthcare settings significantly contribute to the spread of antimicrobial resistance. Inadequate hand hygiene, insufficient sterilization of medical equipment, and the improper isolation of infected patients facilitate the transmission of resistant bacteria. Moreover, the lack of robust infection control measures in community settings exacerbates the problem, allowing resistant strains to spread more widely and rapidly.
By addressing these causes and improving practices around antibiotic use and infection control, we can begin to mitigate the threat posed by antimicrobial resistance.
Consequences of AMR
Health Implications
The health implications of antimicrobial resistance are severe. AMR leads to longer hospital stays, higher medical costs, and increased mortality. Common infections that were once easily treatable with antibiotics are becoming more difficult and sometimes impossible to cure. This leads to prolonged illness and a higher risk of complications and death.
Economic Impact
The economic impact of AMR is substantial. It places a significant financial burden on healthcare systems due to the need for more expensive and intensive treatments. The productivity losses resulting from prolonged illness and disability further strain economies. According to estimates, AMR could cause global economic losses of up to $100 trillion by 2050 if not addressed.
Case Studies and Statistics
Numerous case studies highlight the devastating impact of AMR. For instance, the rise of multi-drug resistant tuberculosis (MDR-TB) has made treatment more complex and less effective. Similarly, the increasing prevalence of methicillin-resistant Staphylococcus aureus (MRSA) infections has led to higher morbidity and mortality rates. Statistics indicate that at least 700,000 deaths globally each year are attributable to drug-resistant infections, a number that is expected to rise dramatically if current trends continue.
Strategies to Combat AMR
Public Awareness and Education
Raising public awareness about AMR and educating people on the responsible use of antibiotics are critical steps in combating the issue. Public health campaigns can help inform individuals about the dangers of misuse and overuse of antibiotics, and the importance of adhering to prescribed treatments.
Stricter Regulations on Antibiotic Use
Implementing stricter regulations on the prescription and use of antibiotics is essential. Policies that limit the use of antibiotics in agriculture and ensure they are prescribed only when necessary in human medicine can significantly reduce the development and spread of resistance.
Infection Prevention and Control Measures
Robust infection prevention and control measures are vital to reducing the spread of AMR. This includes practices such as rigorous hand hygiene, proper sterilization of medical equipment, and the isolation of infected patients. Improving sanitary conditions and access to clean water can also help prevent infections and reduce the need for antibiotics.
Research and Development
Innovations in Antibiotic Research
Investing in the research and development of new antibiotics is crucial to staying ahead of evolving pathogens. Researchers are exploring novel approaches, including bacteriophage therapy, antimicrobial peptides, and other innovative treatments that can effectively combat resistant microorganisms.
Alternative Treatments and Therapies
In addition to developing new antibiotics, alternative treatments and therapies are being investigated. These include the use of probiotics to restore healthy microbiota, immunotherapies to enhance the body’s natural defenses, and the development of vaccines to prevent infections.
Role of Healthcare Professionals
Healthcare professionals play a pivotal role in combating AMR. They must adhere to best practices for prescribing antibiotics, educate patients about the importance of completing their prescribed courses, and implement effective infection control measures. Continuous professional development and training in AMR are essential to ensure healthcare workers are equipped to address this challenge.
Global Collaboration
Importance of International Cooperation
Global collaboration is essential in the fight against antimicrobial resistance. International organizations, governments, healthcare institutions, and individuals must work together to implement effective strategies to combat this threat. Coordinated efforts can help share data, resources, and best practices across borders, enhancing the global response to AMR.
Key Organizations and Initiatives
Several key organizations and initiatives are leading the fight against AMR. The World Health Organization (WHO) has launched the Global Action Plan on Antimicrobial Resistance, which provides a framework for national action plans. The Centers for Disease Control and Prevention (CDC) and the European Centre for Disease Prevention and Control (ECDC) are also actively involved in monitoring and preventing AMR.
Success Stories and Ongoing Efforts
There have been several success stories in the fight against AMR. For example, the implementation of strict infection control measures in hospitals has led to significant reductions in MRSA infections. Ongoing efforts include research into new treatments, public awareness campaigns, and the development of policies to regulate antibiotic use.
Conclusion
Summary of Key Points
Antimicrobial resistance poses a critical threat to global health, with far-reaching consequences for both human and economic well-being. By understanding the causes and implementing comprehensive strategies, we can mitigate the impact of AMR. Public awareness, stricter regulations, robust infection control measures, and investment in research are essential components of this fight.
Call to Action for Individuals and Institutions
It requires concerted efforts from individuals, healthcare professionals, and global entities to ensure the continued effectiveness of antibiotics and the overall health of future generations. Everyone has a role to play in combating antimicrobial resistance, from using antibiotics responsibly to supporting policies and initiatives aimed at reducing AMR.
References and Further Reading
National Institute of Allergy and Infectious Diseases (NIAID) – Antimicrobial Resistance
World Health Organization (WHO) – Antimicrobial Resistance
Centers for Disease Control and Prevention (CDC) – Antibiotic/Antimicrobial Resistance